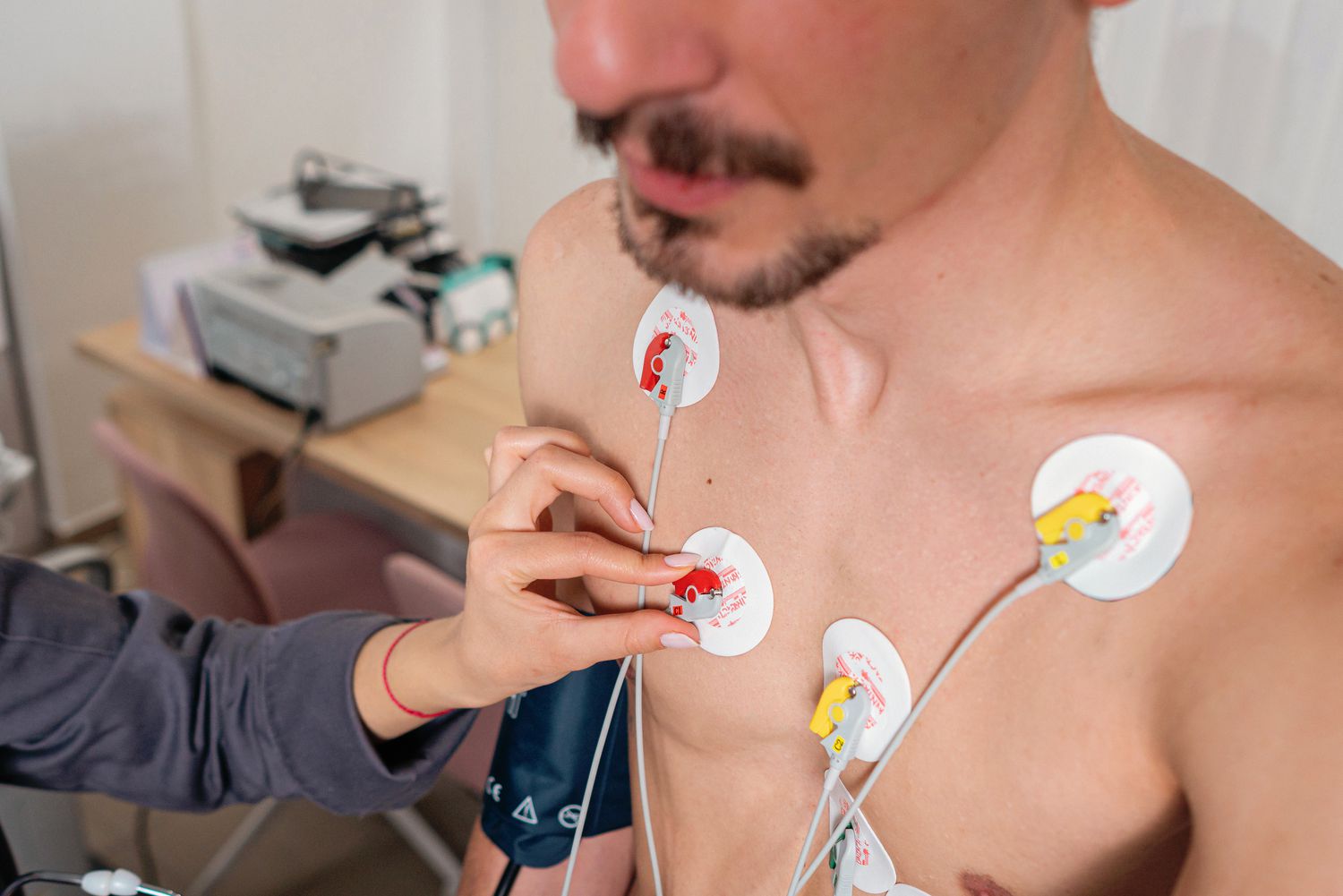
The fundamental importance of the Electrocardiogram (EKG), or ECG as it is often referred to, is frequently obscured by its commonality in medical practice. It is not merely a routine procedure but is, in fact, the initial non-invasive diagnostic modality that provides a graphic and immediate representation of the heart’s electrical life. Without this simple test, the initial evaluation of a patient suspected of having a cardiac-related problem would be significantly delayed and complicated, especially in high-stakes environments like the emergency room. The concept behind it is straightforward yet profoundly effective: the electrical signals that govern the heart’s contractions are measurable on the surface of the skin. Every beat, every depolarization and repolarization, creates a tiny electrical current that is picked up by sticky patches called electrodes, translated by a machine, and displayed as a series of characteristic wavy lines. This tracing acts as a silent language, offering a physician a glimpse into the hidden rhythm and health of the patient’s most vital organ. Its utility is precisely in its quickness and low barrier to entry, making it a ubiquitous, indispensable part of the primary medical assessment globally. The entire procedure, which involves placing these electrodes on the chest, arms, and legs, takes only a few minutes, with absolutely no electricity sent into the body, thereby mitigating any associated risk of electric shock.
The true value of the EKG rests not in its technological complexity, which is relatively minimal compared to modern imaging, but in the critical insights it provides regarding the timing and strength of the heart’s electrical impulse. A normal, healthy heart follows a highly predictable, rhythmic electrical pattern. Deviations from this pattern—subtle or severe—are instantly captured and displayed. The EKG trace is divided into distinct sections, most famously the P wave, the QRS complex, and the T wave, each corresponding to a specific electrical event in the heart’s four chambers. The P wave, for instance, represents the activation of the atria, the heart’s upper chambers, which precedes their contraction. Following swiftly is the QRS complex, the prominent spike which represents the activation of the ventricles, the powerful lower chambers responsible for pumping blood out to the body. Finally, the T wave signifies the electrical recovery phase, or repolarization, as the ventricles prepare for the next beat. The analysis of these waves, including their amplitude, duration, and relative position to one another, forms the foundation of electrocardiography, giving the medical team tangible data on the heart’s electrical consistency and overall function.
Providing Critical Insights into Heart Rate and Rhythm
The EKG trace is divided into distinct sections, most famously the P wave, the QRS complex, and the T wave, each corresponding to a specific electrical event in the heart’s four chambers.
Understanding the temporal and spatial relationships of these electrical events is essential for detecting a wide range of cardiac diseases. For example, by measuring the time between heartbeats, the EKG quickly reveals the heart rate—whether it is unusually fast, known as tachycardia, or unusually slow, referred to as bradycardia. More critically, it is the heart rhythm—the actual signal pattern and consistency between beats—that the EKG truly excels at characterizing. Irregular heartbeats, collectively known as arrhythmias, are precisely what the EKG is designed to detect, with specific patterns pointing toward conditions like atrial fibrillation (AFib) or atrial flutter. Without this electrical mapping, diagnosing these rhythm disturbances, which can lead to complications like stroke or heart failure, would be significantly more challenging and dependent on patient symptoms that may be vague or intermittent. A skilled electrocardiographer, wielding a pair of calipers to precisely measure the intervals on the printout, can deduce the source and nature of a broad array of these rhythm abnormalities with impressive accuracy.
An Unmistakable Signature of Myocardial Infarction
An ECG can diagnose a current or previous heart attack. The patterns on the ECG results can help a healthcare professional learn which part of the heart is damaged.
One of the most immediate and life-saving applications of the EKG is its ability to provide an unmistakable signature of myocardial infarction, commonly known as a heart attack. In the context of an acute event, a significant alteration in the tracing, specifically the ST segment, can indicate that a part of the heart muscle is currently experiencing an inadequate supply of blood and oxygen—a condition called ischemia. The magnitude and location of this deviation on the EKG’s different “leads” (the various electrical viewpoints provided by the electrodes) can literally help a healthcare professional localize and diagnose the infarcted area of the heart, which is critical information for determining the speed and type of intervention needed. Furthermore, an EKG can reveal signs of a previous heart attack that a patient might not have even been aware of, as the scar tissue left by the damage can create distinct, often wide Q waves on the tracing. The EKG thus serves as a powerful retrospective and prospective tool, providing vital clues about the extent of cardiac damage.
Diagnosing Structural Changes in Cardiac Musculature
Many kinds of abnormalities can often be seen on an ECG. They include a previous heart attack, an abnormal heart rhythm, an inadequate supply of blood and oxygen to the heart, and excessive thickening (hypertrophy) of the heart’s muscular walls.
Beyond rhythm and acute damage, the EKG offers valuable, albeit indirect, information regarding the structure and size of the heart’s chambers. Many kinds of abnormalities can be inferred from the tracing, notably excessive thickening (hypertrophy) of the heart’s muscular walls. Conditions such as long-standing high blood pressure or certain heart valve diseases can force the heart to work harder, leading to an enlargement of the muscle mass, particularly in the ventricles. Because a larger muscle mass generates a proportionally larger electrical signal, these structural changes manifest as increased voltage or amplitude in the corresponding deflections on the EKG. While not a direct imaging tool like an echocardiogram, these electrical signs provide an initial, important alert that the heart may be laboring under a mechanical strain, necessitating further investigation. Abnormalities can also sometimes suggest the presence of aneurysms—bulges that develop in weakened areas of the heart’s walls, often as a result of prior attack.
Assessing Blood and Oxygen Supply During Exertion
An EKG done while you’re having chest pain symptoms can help your care team learn whether reduced blood flow to the heart is the cause.
The standard resting EKG provides a momentary “snapshot” of the heart’s activity over a very short time, which is usually only about one minute. However, many heart problems, particularly those stemming from blocked or narrowed coronary arteries, only manifest when the heart is placed under stress. To capture these exertion-dependent problems, the EKG can be integrated into a stress test (also known as a treadmill test or exercise tolerance test). During this test, a patient walks on a treadmill or cycles on a stationary bike while their heart’s electrical activity is continuously monitored via the electrodes. The key here is that reduced blood flow to the heart will become apparent as the heart rate increases and the muscle demands more oxygen, often leading to alterations in the ST segment or the onset of symptoms like chest pain or shortness of breath. This variation of the test is crucial because it literally reveals problems that lie in wait when the heart is resting, providing evidence of coronary artery disease that a resting EKG might completely miss.
Monitoring the Efficacy of Therapeutic Interventions
Your doctor might also use an electrocardiogram to see: How well heart medications or treatments (such as pacemakers) are working.
The clinical utility of the EKG extends well beyond initial diagnosis; it is an indispensable monitoring tool throughout a patient’s treatment journey. After a patient has been diagnosed with a heart condition, physicians frequently rely on subsequent EKGs to monitor the efficacy of heart medications, particularly those used to control rhythm disturbances, known as antiarrhythmics. By tracking changes in the P-R interval or the Q-T interval—the time measurements between specific waves—doctors can assess how well a drug is stabilizing the heart’s electrical system and whether it is causing any adverse electrical effects. Furthermore, for patients with implanted devices like pacemakers, the EKG is used to verify that the device is functioning correctly and delivering its electrical impulses as programmed, ensuring the pacing is captured and conducted normally by the heart muscle. In this capacity, the EKG serves as an early warning system, providing a quick check on the internal mechanics of ongoing treatment.
The Subtle Art of Interpreting the Electrical Vectors
The direction in which the waves point indicates whether electricity is moving towards or away from a particular lead.
The interpretation of the EKG requires a detailed understanding of the heart’s electrical conduction system and how its activity is projected onto the body’s surface. The standard 12-lead EKG uses ten cables to generate twelve distinct electrical views, or vectors, of the heart. The general electrical impulse normally travels in a predictable, downward diagonal direction, originating in the sinoatrial (SA) node and propagating throughout the muscle. The principle here is simple yet powerful: electrical activity moving toward a lead causes an upward deflection on the graph, while activity moving away causes a downward deflection. This complex spatial mapping allows the clinician to not only identify a problem but to localize it to a specific area, such as the left ventricle or the interventricular septum. Consequently, an inverted or oddly shaped wave in a single lead may signal an issue that requires further attention, providing a precise geographical reference for the underlying cardiac pathology.
Distinguishing Electrical Instability from Mechanical Issues
The ECG recording plays an irreplaceable role in diagnostics of various cardiovascular diseases.
It is crucial to recognize that the EKG is a tool for measuring electrical activity and not a direct measure of the heart’s mechanical pumping efficiency or the detailed anatomy of its valves, which is the domain of tests like the echocardiogram. However, the electrical record is a powerful surrogate for overall cardiac health. The EKG recording plays an irreplaceable role in diagnostics because certain conditions, particularly all forms of arrhythmias, are completely reliant on the EKG for their definitive identification. Furthermore, monitoring the QT interval prolongation, which is an independent risk factor for dangerous ventricular arrhythmias, can be detected exclusively from an EKG trace. Thus, while it has limitations—it won’t depict decreased blood flow if the patient is not currently in distress—it remains the “gold standard” for characterizing the heart’s rhythm and electrical stability, providing a clear and immediate guide for urgent and long-term therapeutic choices.
A Foundational Element of Preoperative Assessment
An ECG serves as an integral part of preoperative assessment of patients undergoing non-cardiac surgery.
The widespread application of the EKG also extends to its use as an integral part of preoperative assessment for patients undergoing non-cardiac surgery. Before a major surgical procedure, especially in older patients or those with pre-existing risk factors like diabetes or hypertension, it is paramount to establish a baseline tracing of the heart’s function. This simple EKG screens for any underlying, potentially silent, heart conditions—such as an undiagnosed arrhythmia or signs of previous damage—that could complicate the surgery or recovery under anesthesia and surgical stress. Having this baseline record is essential for risk stratification and for providing a necessary point of comparison against future EKGs should a cardiac event occur during or after the procedure. It is a fundamental safety check, ensuring that the cardiac machinery is in the best possible state before being subjected to the rigors of an operation.
The Endurance of a Simple, Essential Diagnostic
The electrocardiogram is the oldest and most enduring tool of the cardiologist.
The EKG, which was first invented in 1902 by Willem Einthoven, stands as the oldest and most enduring tool of the cardiologist, a testament to the robustness and elegance of its initial design. Despite the advent of sophisticated, high-resolution imaging and continuous monitoring technologies, the EKG retains its indispensable position in almost every healthcare setting globally. Its ease of use, non-invasiveness, speed, and low cost make it the perfect initial test to quickly establish or rule out many of the most critical and time-sensitive cardiac issues. It is a fundamental piece of the diagnostic puzzle, providing the essential electrical context needed to inform the need for subsequent, more complex tests. For the physician in the emergency room dealing with a patient experiencing chest pain, the EKG remains the first line of defense, offering rapid, actionable intelligence.
