Breathing patterns offer early warnings. Shortness of breath returns despite consistent use of medication. Patients might notice increased effort during simple tasks. Climbing stairs may become exhausting again. Breathing could feel labored even at rest. The sensation doesn’t always involve chest pain. Oxygen exchange may be impaired by fluid buildup. This issue is common in congestive heart failure relapse. The lungs struggle when blood isn’t pumped efficiently.
Swelling in the ankles or feet begins to increase gradually
Fluid retention reflects cardiac strain. Swelling in the ankles or feet begins to increase gradually. Socks might leave deeper indentations. Shoes may feel tighter during the evening. The swelling could progress toward the lower legs. Medication like diuretics might become less effective. The kidneys retain sodium and water under poor circulation. This often suggests worsening left ventricular function. Edema is not always painful but should be noted carefully.
Heart rate feels erratic or too slow despite being medicated
Pulse irregularities can indicate treatment failure. Heart rate feels erratic or too slow despite being medicated. Some medications aim to control arrhythmias. Beta-blockers may lose their effectiveness with time. Patients might feel palpitations or skipped beats. Others notice bradycardia causing dizziness or fatigue. A stable rhythm is essential for consistent cardiac output. Monitoring at home can help detect early changes. Sudden shifts should always be reported.
Fatigue becomes noticeable even during minor physical activity
Low energy levels may reflect inadequate control. Fatigue becomes noticeable even during minor physical activity. Walking short distances can feel difficult. Simple chores may require rest breaks. The heart might not be delivering enough oxygen. Blood flow can drop due to reduced ejection fraction. Some medications need time to adjust dosage. Persistent tiredness signals the body is compensating. Reassessment may be necessary to improve circulation.
Chest discomfort reappears or worsens during daily tasks
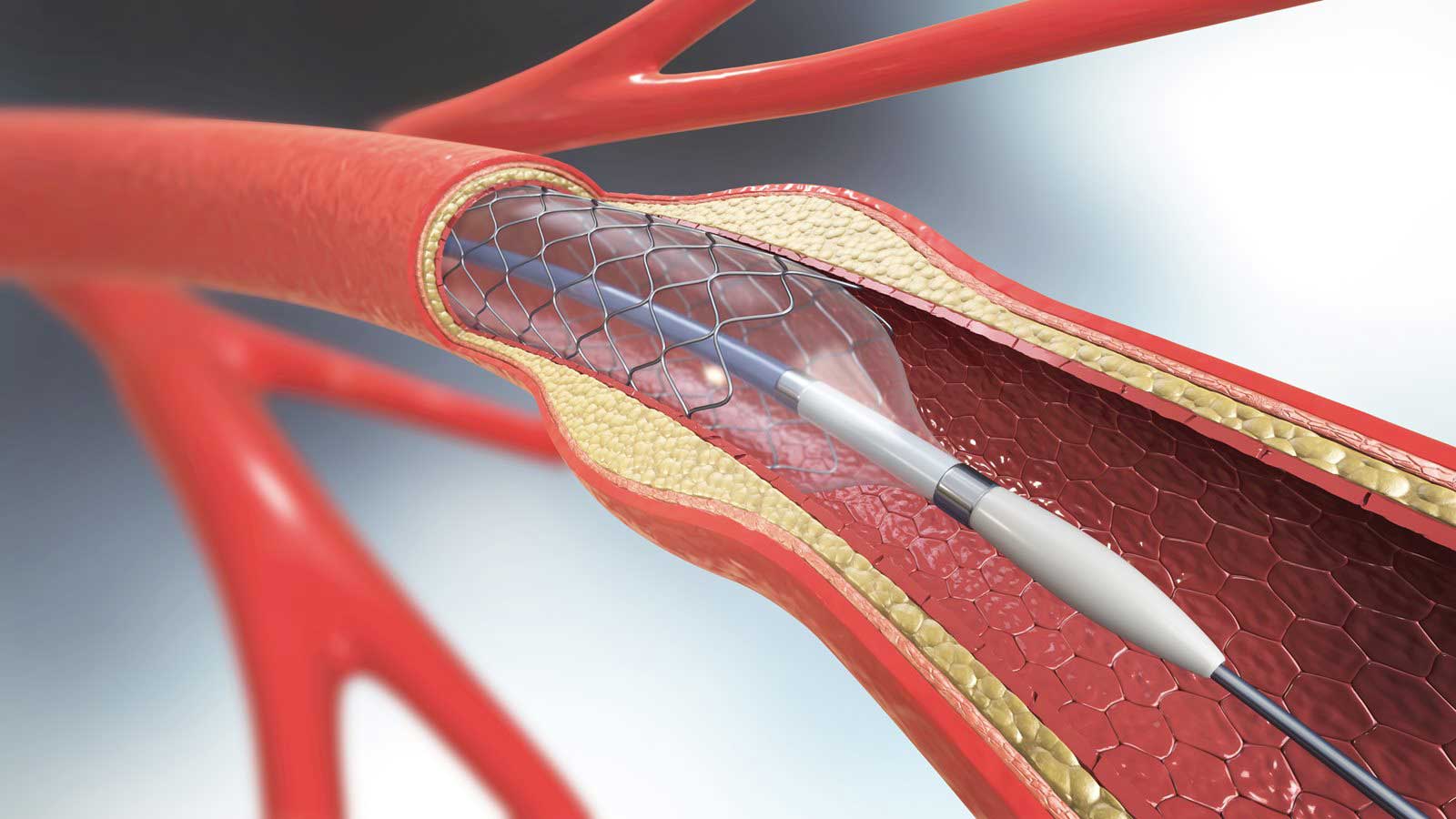
Pain symptoms can reemerge subtly. Chest discomfort reappears or worsens during daily tasks. Pressure or heaviness may feel familiar. It might occur during stress or exertion. Nitrates or calcium blockers may lose efficacy. Coronary arteries could be narrowing further. This pain doesn’t always mimic a classic heart attack. Radiating discomfort may extend to shoulders or neck. Changes should be evaluated with updated imaging or stress testing.
Sudden weight gain of several pounds in a short time span
Body weight shifts rapidly during decompensation. Sudden weight gain of several pounds in a short time span. This is not always related to diet. The body may be retaining fluids aggressively. Daily weight tracking becomes vital in heart failure. Gaining more than two pounds overnight is concerning. Increased abdominal girth might follow quickly. The liver and other organs can also become congested. Diuretics may need adjustment immediately.
Dizziness occurs more frequently after standing or walking
Blood pressure medication can affect stability. Dizziness occurs more frequently after standing or walking. The body’s compensatory reflexes may slow down. Hypotension might result from overtreatment. ACE inhibitors or vasodilators sometimes overshoot their effect. Reduced pressure can limit brain perfusion. Standing from bed or chair might trigger lightheadedness. The symptom may lead to falls or fainting. Doctors must reassess dosing and timing.
Cough develops that doesn’t improve and interrupts sleep
Respiratory changes may link back to cardiac causes. Cough develops that doesn’t improve and interrupts sleep. It often worsens when lying flat. Fluid may back up into the lungs. ACE inhibitors themselves can also cause chronic dry cough. Productive coughs suggest more serious fluid overload. Nighttime symptoms usually indicate pulmonary involvement. Elevating the head during sleep might bring relief. Nonetheless, the underlying issue remains cardiovascular.
Blood pressure readings begin to trend back toward previous levels
Baseline monitoring shows relapse patterns. Blood pressure readings begin to trend back toward previous levels. Initially controlled values may begin creeping up. Systolic numbers may rise gradually without noticeable symptoms. Hypertension strains the heart muscle further. Medication adherence should be confirmed first. If compliant, dose modification may follow. Dietary sodium intake should also be reviewed. The return of high pressure is rarely isolated.
Mood changes occur alongside physical symptoms of cardiac instability
Emotional shifts can accompany medication failure. Mood changes occur alongside physical symptoms of cardiac instability. Patients may feel unusually irritable or withdrawn. Anxiety can increase when breathing worsens. Depression is common in poorly controlled heart conditions. Lack of progress leads to frustration. Fatigue often amplifies negative emotions. Doctors sometimes miss these signals during routine visits. Mental health support must run parallel to physical treatment.
