Understanding heart failure can be tricky. It’s not when the heart stops. Instead, it means the heart struggles. It can’t pump blood effectively. Blood delivery to the body slows. This impacts many vital organs. The body doesn’t get enough oxygen. It doesn’t receive enough nutrients. This condition can worsen over time. It can become a chronic issue.
The Heart’s Pumping Action
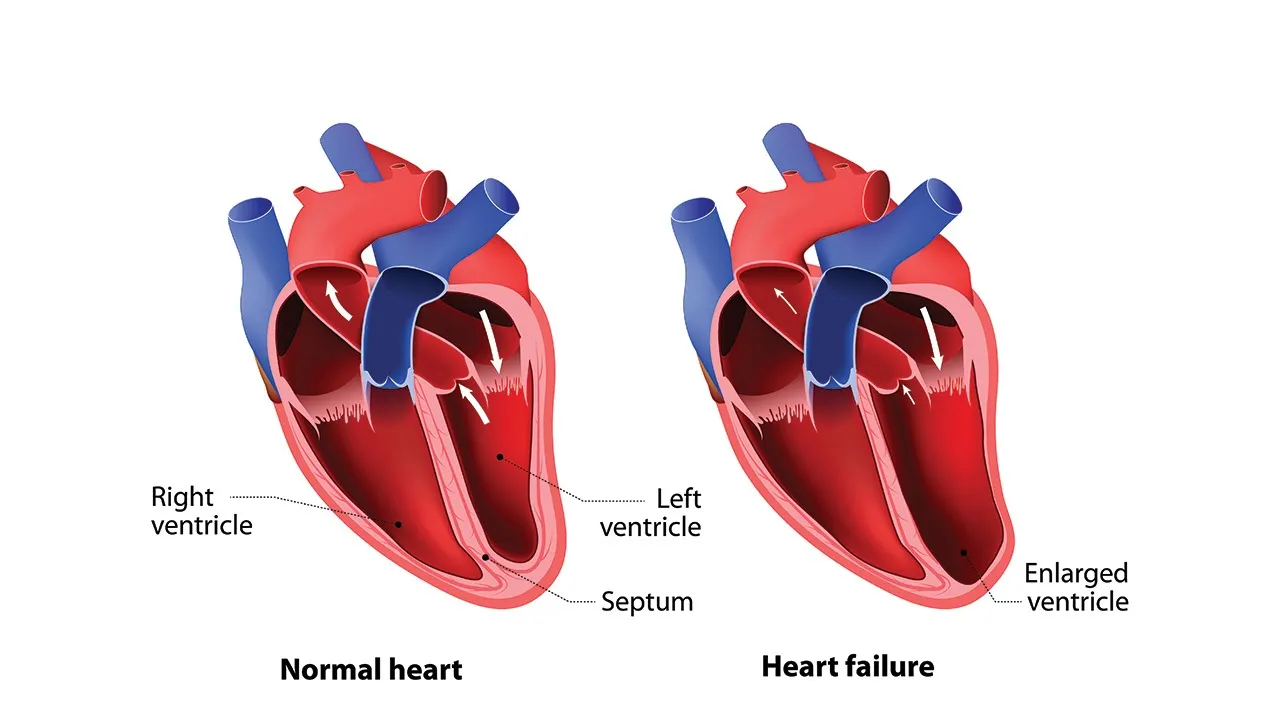
Your heart is a powerful pump. It works tirelessly every second. It has four distinct chambers. Two atria, two ventricles. They work in perfect rhythm. Blood enters the atria first. Then it moves to the ventricles. The ventricles pump blood out. The right side sends blood to lungs. The left side sends blood to the body. Heart failure disrupts this process. The pumping action becomes weak.
Left-Sided Heart Failure
This is the most common type. The left ventricle weakens. It struggles to pump blood out. Blood backs up into the lungs. This causes fluid buildup. Doctors call this pulmonary congestion. Symptoms include shortness of breath. This worsens with activity. Lying flat can make it harder. A persistent cough may develop. Sometimes, wheezing is present. Swelling in legs may occur.
Right-Sided Heart Failure
The right ventricle is affected here. It can’t pump blood to the lungs. Blood backs up in the body. This causes fluid retention. Swelling appears in the legs. Ankles and feet are common sites. The abdomen may also swell. You might feel bloated. Nausea or loss of appetite occurs. This type often follows left-sided. But it can happen alone. Lung conditions can cause it.
Systolic Heart Failure
This type impacts pumping strength. The heart muscle weakens. It can’t contract forcefully enough. It struggles to eject blood. Less blood leaves the ventricle. This leads to reduced circulation. It’s often due to heart attacks. High blood pressure also plays a role. The ejection fraction is low. Doctors measure this percentage. It indicates pumping efficiency.
Diastolic Heart Failure
Here, the heart muscle stiffens. It can’t relax properly. The ventricles don’t fill enough. Even with good pumping strength. Less blood enters the chambers. So, less blood is pumped out. High blood pressure is a common cause. Diabetes can also contribute. The ejection fraction is often normal. But the filling is impaired. This type is also very serious.
Common Causes of Failure
Many conditions lead to heart failure. Coronary artery disease is primary. Narrowed arteries reduce blood flow. This weakens the heart muscle. High blood pressure is another factor. It forces the heart to work harder. Over time, it gets tired. Heart attacks cause muscle damage. This impairs pumping ability. Diabetes also increases risk. Valve problems hinder blood flow. Irregular heart rhythms can too.
Symptoms Are Varied
Symptoms develop gradually often. Shortness of breath is common. Fatigue and weakness occur. Swelling in legs or ankles appears. A persistent cough may bother you. Especially at night or lying down. Rapid or irregular heartbeat is possible. Abdominal swelling may occur. Lack of appetite can be an issue. Weight gain from fluid is common. Dizziness or confusion might happen.
Diagnosis Involves Tests
Doctors use various methods. A physical exam is the first step. They listen to your heart and lungs. Blood tests check kidney function. They measure certain hormones. An echocardiogram is crucial. It shows heart structure and function. It measures ejection fraction. An ECG checks electrical activity. Chest X-rays show fluid in lungs. Sometimes, MRI or CT scans are done.
Medications Help Management
Medicines are vital for treatment. They improve heart function. They reduce symptoms significantly. Diuretics remove excess fluid. ACE inhibitors relax blood vessels. Beta-blockers slow heart rate. They improve pumping action. Aldosterone antagonists are also used. These reduce fluid and protect heart. Other drugs target specific issues. Taking meds as prescribed is critical.
Lifestyle Changes Are Crucial
You play a big role in care. Limit sodium intake strictly. This reduces fluid retention. Follow a heart-healthy diet. Eat fruits, vegetables, whole grains. Avoid processed foods and unhealthy fats. Maintain a healthy weight. Regular, moderate exercise helps. Quit smoking entirely. Limit alcohol consumption. These changes support treatment. They improve quality of life.
Fluid Monitoring at Home
Daily weighing is important. It helps track fluid retention. Weigh yourself every morning. Use the same scale always. Wear similar clothing each time. Report sudden weight gain. More than 2-3 pounds in a day. Or 5 pounds in a week. This indicates fluid buildup. Your doctor can adjust medication. This prevents worsening symptoms. Be vigilant about your weight.
Device Therapies Exist
Some patients need advanced care. Pacemakers regulate heart rhythm. They can improve pumping efficiency. Implantable defibrillators prevent sudden death. They deliver shocks for dangerous rhythms. Cardiac resynchronization therapy (CRT) helps. It coordinates heart contractions better. These devices are surgically implanted. They offer significant benefits. Your doctor will assess suitability.
Advanced Treatment Options
For severe cases, other options exist. Heart valve repair or replacement. It fixes faulty valves. Coronary bypass surgery helps. It improves blood flow to heart. A ventricular assist device (VAD). It helps pump blood from the heart. It can be a bridge to transplant. Heart transplant is the last resort. It replaces the failing heart. These are major, complex procedures.
Living with Heart Failure
It’s a chronic condition. Management is lifelong. Regular doctor visits are vital. Follow all instructions carefully. Monitor your symptoms daily. Report changes promptly. Join a support group. Connect with others facing similar issues. Learn as much as you can. Empower yourself with knowledge. With proper care, life can be good. Focus on managing your health.
